Breast Cancer Main Page
Colon Cancer Main Page
Skin Cancer Main Page
Mesothelioma Cancer
Prostate Cancer Main Page
Gynecologic Cancers Main Page
Lung Cancer Main Page |
What Is Lung Cancer?
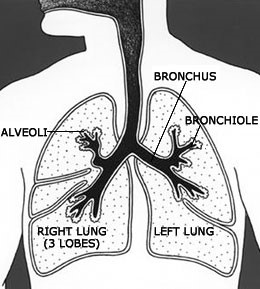
Image of the thorax with a diagram of lungs, alveoli, bronchus, and bronchiole. The right lung has three segments or lobes and the left lung has two.
Cancer is a disease in which cells in the body grow out of control. When cancer starts in the lungs, it is called lung cancer.
Lung cancer begins in the lungs and may spread to lymph nodes or other organs in the body, such as the brain. Cancer from other organs also may spread to the lungs. When cancer cells spread from one organ to another, they are called metastases.
Lung cancers usually are grouped into two main types called small cell and non-small cell. These types of lung cancer grow differently and are treated differently. Non-small cell lung cancer is more common than small cell lung cancer.
|
 |
What Are the Risk Factors?
Need Help Quitting?
- Visit smokefree.gov

- Call 1 (800) QUIT-NOW
- Text “QUIT” to 47848 from your cell phone
Research has found several risk factors that may increase your chances of getting lung cancer.
Smoking
Cigarette smoking is the number one risk factor for lung cancer. In the United States, cigarette smoking causes about 90% of lung cancers. Using other tobacco products such as cigars or pipes also increases the risk for lung cancer. Tobacco smoke is a toxic mix of more than 7,000 chemicals. Many are poisons. At least 70 are known to cause cancer in people or animals.
People who smoke are 15 to 30 times more likely to get lung cancer or die from lung cancer than people who do not smoke. Even smoking a few cigarettes a day or smoking occasionally increases the risk of lung cancer. The more years a person smokes and the more cigarettes smoked each day, the more risk goes up.
People who quit smoking have a lower risk of lung cancer than if they had continued to smoke, but their risk is higher than the risk for people who never smoked. Quitting smoking at any age can lower the risk of lung cancer.
Smoking can cause cancer almost anywhere in the body. Smoking causes cancer of the mouth, nose, throat, voicebox (larynx), esophagus, bladder, kidney, pancreas, cervix, stomach, blood, and bone marrow (acute myeloid leukemia).

Secondhand Smoke
Smoke from other people's cigarettes, pipes, or cigars (secondhand smoke) also causes lung cancer. When a person breathes in secondhand smoke, it is like he or she is smoking. In the United States, two out of five adults who don't smoke and half of children are exposed to secondhand smoke, and about 3,000 people who never smoked die from lung cancer due to secondhand smoke every year.
Radon
Radon is a naturally occurring gas that comes from rocks and dirt and can get trapped in houses and buildings. It cannot be seen, tasted, or smelled. According to the U.S. Environmental Protection Agency (EPA), radon causes about 20,000 cases of lung cancer each year, making it the second leading cause of lung cancer. Nearly one out of every 15 homes in the U.S. is thought to have high radon levels. The EPA recommends testing homes for radon and using proven ways to lower high radon levels.
radon causes about 20,000 cases of lung cancer each year, making it the second leading cause of lung cancer. Nearly one out of every 15 homes in the U.S. is thought to have high radon levels. The EPA recommends testing homes for radon and using proven ways to lower high radon levels.
Other Substances
Examples of substances found at some workplaces that increase risk include asbestos, arsenic, diesel exhaust, and some forms of silica and chromium. For many of these substances, the risk of getting lung cancer is even higher for those who smoke.
Family History
Your risk of lung cancer may be higher if your parents, brothers or sisters, or children have had lung cancer. This could be true because they also smoke, or they live or work in the same place where they are exposed to radon and other substances that can cause lung cancer.
Radiation Therapy to the Chest
Cancer survivors who had radiation therapy to the chest are at higher risk of lung cancer. Patients at highest risk include those treated for Hodgkin disease and women with breast cancer treated with radiation after a mastectomy (but not a lumpectomy).
Diet
Scientists are studying many different foods and dietary supplements to see whether they change the risk of getting lung cancer. There is much we still need to know. We do know that smokers who take beta-carotene supplements have increased risk of lung cancer. For more information, visit Lung Cancer Prevention.
Also, arsenic in drinking water (primarily from private wells) can increase the risk of lung cancer. For more information, visit the EPA's Arsenic in Drinking Water.
What Are the Symptoms?
Different people have different symptoms for lung cancer. Some people have symptoms related to the lungs. Some people whose lung cancer has spread to other parts of the body (metastasized) have symptoms specific to that part of the body. Some people just have general symptoms of not feeling well. Most people with lung cancer don't have symptoms until the cancer is advanced. Lung cancer symptoms may include—
- Coughing that gets worse or doesn't go away.
- Chest pain.
- Shortness of breath.
- Wheezing.
- Coughing up blood.
- Feeling very tired all the time.
- Weight loss with no known cause.
Other changes that can sometimes occur with lung cancer may include repeated bouts of pneumonia and swollen or enlarged lymph nodes (glands) inside the chest in the area between the lungs.
These symptoms can happen with other illnesses, too. If you have some of these symptoms, talk to your doctor, who can help find the cause.
What Can I Do to Reduce My Risk?
Need Help Quitting?
- Visit smokefree.gov

- Call 1 (800) QUIT-NOW
- Text “QUIT” to 47848 from your cell phone
You can help lower your risk of lung cancer in the following ways—
- Don’t smoke. Smoking causes about 90% of lung cancer deaths in men and almost 80% of lung cancer deaths in women in the United States. The most important thing you can do to prevent lung cancer is to not start smoking, or to quit if you smoke.
- Avoid secondhand smoke. Smoke from other people’s cigarettes, pipes, or cigars is called secondhand smoke. Make your home and car smoke-free.
- Get your home tested for radon. The U.S. Environmental Protection Agency
 recommends that all homes be tested for radon.
recommends that all homes be tested for radon.
- Be careful at work. Health and safety guidelines in the workplace can help workers avoid carcinogens—things that can cause cancer.
Related Links
What Screening Tests Are There?

Screening means testing for a disease when there are no symptoms or history of that disease. Doctors recommend a screening test to find a disease early, when treatment may work better.
means testing for a disease when there are no symptoms or history of that disease. Doctors recommend a screening test to find a disease early, when treatment may work better.
The only recommended screening test for lung cancer is low-dose computed tomography (also called a low-dose CT scan, or LDCT). In this test, an X-ray machine scans the body and uses low doses of radiation to make detailed pictures of the lungs.
Who Should Be Screened?
The U.S. Preventive Services Task Force recommends yearly lung cancer screening with LDCT for people who—
yearly lung cancer screening with LDCT for people who—
- Have a history of heavy smoking, and
- Smoke now or have quit within the past 15 years, and
- Are between 55 and 80 years old.
Heavy smoking means a smoking history of 30 pack years or more. A pack year is smoking an average of one pack of cigarettes per day for one year. For example, a person could have a 30 pack-year history by smoking one pack a day for 30 years or two packs a day for 15 years.
Risks of Screening
Lung cancer screening has at least three risks—
- A lung cancer screening test can suggest that a person has lung cancer when no cancer is present. This is called a false-positive result. False-positive results can lead to follow-up tests and surgeries that are not needed and may have more risks.
- A lung cancer screening test can find cases of cancer that may never have caused a problem for the patient. This is called overdiagnosis. Overdiagnosis can lead to treatment that is not needed.
- Radiation from repeated LDCT tests can cause cancer in otherwise healthy people.
That is why lung cancer screening is recommended only for adults who have no symptoms but who are at high risk for developing the disease because of their smoking history and age.
If you are thinking about getting screened, talk to your doctor. If lung cancer screening is right for you, your doctor can refer you to a high-quality treatment facility.
The best way to reduce your risk of lung cancer is to not smoke and to avoid secondhand smoke. Lung cancer screening is not a substitute for quitting smoking.
When Should Screening Stop?
The Task Force recommends that yearly lung cancer screening stop when the person being screened—
- Turns 81 years old, or
- Has not smoked in 15 years, or
- Develops a health problem that makes him or her unwilling or unable to have surgery if lung cancer is found.
Lung Cancer Statistics
More people in the United States die from lung cancer than any other type of cancer. This is true for both men and women. For more information, visit Cancer Among Men and Cancer Among Women.
In 2010 (the most recent year numbers are available)—
- 201,144 people in the United States were diagnosed with lung cancer, including 107,164 men and 93,980 women.*†
- 158,248 people in the United States died from lung cancer, including 87,698 men and 70,550 women.*†
*Incidence counts cover about 97% of the U.S. population; death counts cover about 100% of the U.S. population. Use caution when comparing incidence and death counts.
†Source: U.S. Cancer Statistics Working Group. United States Cancer Statistics: 1999–2010 Incidence and Mortality Web-based Report. Atlanta (GA): Department of Health and Human Services, Centers for Disease Control and Prevention, and National Cancer Institute; 2013. Available at: http://www.cdc.gov/uscs.